The characteristics of Fetal Alcohol Spectrum Disorder vary from child to child (and adult to adult), depending on both the amount of alcohol exposure in utero and the specific point in gestation at which exposure occurred. This poses a problem for diagnosticians as there can be a lack of observable signs and biological markers on which to base a diagnosis. Compounding this diagnostic challenge is the sense of shame mothers may feel, and their consequent reluctance to accurately report alcohol use in pregnancy.
Consequently, clinicians typically rely upon a set of behavioural characteristics to reach a diagnosis of FASD in a child or adult. These include:
- Memory difficulties
- Impulsivity, distractibility
- Inability to action instructions
- Difficulty with abstract thinking
- Slower auditory pace
- Cognitive processing deficits
- Developmental delays
- Inability to predict outcomes and understand consequences
Diagnosing FAS:
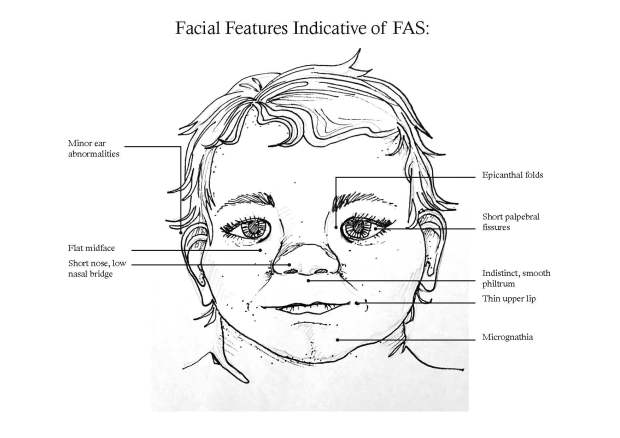
Fetal Alcohol Syndrome is the more severe manifestation of FASD and is diagnosed based on a combination of central nervous system abnormality, growth and developmental indicators and facial dysmorphia. The use of morphological features in diagnosis makes the clinician’s task more straightforward, and diagnosis can be reached in young infants. Facial abnormalities now accepted by the global medical community as being indicative of FAS are shown below:
Facial Features Associated with FAS:
- Short palpebral fissures (the vertical amount of eyeball exposed between eyelids, often simply expressed as small eyes)
- Flat midface
- Short nose
- Indistinct philtrum (the groove running from the base of the nose to the top of the upper lip)
- Thin upper lip
- Epicanthal folds (skin folds of the upper eyelid covering the inner corner of the eye)
- Low nasal bridge
- Minor ear anomalies
- Micrognathia (undersized jaw)


Both FASD and FAS require a coordinated multi-disciplinary health care team including child psychologists, highly trained speech pathologists and paediatricians to assess the child to properly assess facial features and behavioural characteristics to determine if they are in fact due to Fetal Alcohol Spectrum Disorder.
Implications of Diagnosis:
The ambiguity inherent in diagnosis, coupled with the comparative newness of the condition, facial variation due to ethnicity and the variety of symptoms and signs FAS and FASD present poses a problem for sufferers. Diagnosis is important as it is the first step towards getting assistance, be it cognitive behavioural therapy or social supports.
The risk is that without a clear and accepted test clinicians may be under diagnosing FASD, in fact it is generally accepted that this is the case. Misconceptions and a lack of knowledge amongst primary care providers mean that many assume a child will only have FASD if the mother is an alcoholic.
This means children with less severe manifestations of the syndrome are at risk of not receiving the support from government agencies to maximise their potential development as they progress through the school system.
For further information on diagnosing FASD watch the following interview with Dr Doug Shelton, Director of Children’s Health at Gold Coast Health, one of only 2 diagnostic centres in Australia:
So far we have spoken about FASD in Australia. The symptoms of FASD and the difficulty diagnosing the condition are a worldwide health issue. South Africa has the highest rates of diagnosed FASD in the world. To understand the extent of the problem in that region you may like to watch an ABC News report from 2011 which documents one sufferers signs and symptoms and talks about FASD in a different country:
References:
Hayes L, D’Antoine H, Carter M. Chapter 20 – Addressing Fetal Alcohol Spectrum Disorder in Aboriginal Communities, p 355-371. In: Pat Dudgeon, Helen Milroy, Roz Walker.Working together: Aboriginal and Torres Strait Islander mental health and wellbeing principles and practice. 2nd edition. Telethon Kids Institute, Kulunga Aboriginal Research Development Unit, Department of the Prime Minister and Cabinet (Australia).
Payne J. Elliott E, D’Antoine H, O’Leary C, Mahony A, Hann E et al. Health Professionals Knowledge, practice and opinions about fetal alcohol syndrome and alcohol consumption in pregnancy. Australia and New Zealand Journal of Public Health 2005; 29(6): 558-564.
Department of Health and Human Services. National Centre on Birth Defects and Developmental Disabilities; Fetal Alcohol Syndrome – Guidelines for Referral and Diagnosis. Department of Health and Human Services. Washington 2004.
Available from:
Click to access FAS_guidelines_accessible.pdf
Image 1: Drawn by Anna Faunt.
Image 2: http://drugster.info/medic/term/fetal-alcohol-syndrome-diagnosis
Image 3: http://alcoholpregnancy.telethonkids.org.au/understanding-fasd/what-is-fasd/